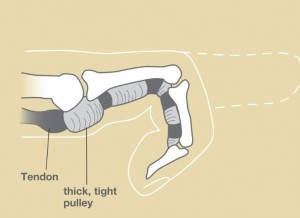
Trigger finger is a condition affecting any of the fingers or thumb in the hand — not just the index finger. Symptoms occur when there is catching between the flexor tendons of the hand and the sheath which surrounds the tendons. Instead of gliding smoothly through the sheath, the tendons can meet resistance within the tight sheath, which can be painful and cause the finger to be stiff. Some patients report “catching” or “clicking” of the finger with movement. This can make the hand difficult to use. Some patients may feel a tender nodule or “bump” in the palm at the base of the finger. In worse cases, the finger can become stuck or “locked” in flexion, requiring the person the straighten the finger with the other hand. This “unlocking” of the finger can be very painful. These symptoms are often worse in the morning.
What causes trigger finger?
The cause of trigger finger is unknown in most cases. Repetitive, forceful gripping with the hand or trauma may contribute. Sometimes rheumatoid arthritis (RA), diabetes, gout, and thyroid disorders are associated.
Who is at risk for trigger finger?
Trigger finger is 3 times more common in females than males. It typically occurs in people between 40 and 60 years of age. Diabetics and patients with RA have a higher risk. Trigger finger can occur in any finger, and it is also common in the thumb.
Children may also have a trigger finger, however, this is much less common. “Congenital trigger thumb” is occasionally diagnosed in infants who cannot fully straighten the end of the thumb.
How is trigger finger diagnosed?
Trigger finger can be diagnosed by careful evaluation by a physician. Laboratory tests, x-rays, ultrasound, and MRI are usually not necessary.
What are the treatment options?
Non-operative treatment is tried first. Using a splint at night can reduce swelling and decrease triggering. Resting the hand may also help. Oral anti-inflammatory medications such as Ibuprofen, Naproxen, and Tylenol can help reduce pain and inflammation. A steroid injection (cortisone shot) can fix the problem in many patients.
If this does not help, surgery may be recommended. Trigger finger release surgery can be performed to improve the tendon range of motion. During this procedure, the tight sheath (the A1 pulley) is opened through a small incision in the palm and this allows the tendons to glide smoothly. Local anesthesia is typically used, and most patients do not need to be put to sleep for the procedure.
What is the recovery from surgery?
The surgery is performed in a surgery center with local anesthesia. A Valium pill can be used to help with relaxation. Patients may use their hands for light activities. I encourage gentle finger or thumb range of motion to reduce stiffness. Most people can return to light duty work in a few of days. Normal use of the hand is resumed as comfort permits. The soft surgical bandage can be removed after about 5 days. Afterwards the wound should be covered with a light dressing, such as a band-aid. The skin sutures are removed in clinic in 10-14 days. I typically recommend avoiding heavy use with the hand for approximately 3-4 weeks after surgery.
What are the results from surgery?
Free gliding of the tendons is noticed soon after surgery. Most patients are very satisfied with their outcome. However, some patients report mild soreness in the palm and stiffness of the digit, which often improve over a few weeks or months. People with hand arthritis are more prone to hand stiffness. Occasionally hand therapy is recommended to improve range of motion and decrease pain. Recurrence of the finger triggering after surgery is very uncommon.
What are the complications from surgery?
No surgery is risk-free. However, major complications from trigger finger release are uncommon. Possible complications include pain, persistent symptoms, bleeding, infection, finger stiffness, wound healing problems and damage to the tendons or sensory nerves. Other complications are possible but are uncommon.
The image and video are provided by the American Society for Surgery of the Hand