What is a Trigger Finger?
Many patients are under the impression that the pointer finger is the “trigger finger.” However, in a hand surgery clinic, a trigger finger has nothing to do with guns or firearms. A trigger finger is a common hand condition in which a finger catches, locks, or “triggers,” during range of motion. This can occur in any of the fingers, including the thumb! Actually, the ring finger is the most common trigger finger.
In normal functioning of the hand, the tendons which pull the finger into flexion glide smoothly in the palm. This tendon movement is guided by a tunnel from the palm into the fingertip. Normally the tendon moves unrestricted and pain-free within the tunnel. If there is thickening of the tissues or swelling in the area, however, the tendon rubs against the surface of the tunnel. This increased mechanical friction can result in limited finger range of motion, increased finger swelling, and pain. Classically, the finger gets stuck in flexion when the patient makes a fist. In most cases, the patient can straighten out the finger quickly and the finger will pop open. In some cases the finger locks in flexion, and it requires the patient to use their other hand to straighten the bent finger. The triggering or locking episodes can be very painful, but in some cases the triggering is only mildly uncomfortable for some patients. Prolonged trigger fingers can result in limited finger range of motion and reduced hand function.
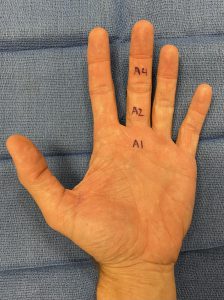
The tunnel through which the flexor tendons glide is called the flexor tendon sheath. The sheath is made up of several important pulleys which keep the tendon in place while the finger is moving. This system of tendons and pulleys is similar to how a fishing line is held to a fishing rod. The first pulley in the palm, the A1 pulley, is usually the location of the problem in trigger fingers. The A1 pulley area is where most patients have pain. The A2 and A4 pulleys in the finger are functionally important pulleys, and are usually not a problem in this condition. Each finger has two flexor tendons, called the FDP and FDS tendons. The thumb only has one flexor tendon, the FPL tendon.
Why does a trigger finger occur?
In most patients, there is not a clear explanation for why a trigger finger develops. The known risk factors for developing a trigger finger include diabetes, thyroid disorder, rheumatoid arthritis, and gout. Repetitive, forceful gripping and squeezing with the hand as well as trauma may also be risk factors. Patients with carpal tunnel syndrome are also prone to developing trigger fingers either before or after carpal tunnel surgery.
What are the treatments for trigger fingers?
Trigger fingers were first described by French physician Dr. Notta in 1850. At that time, there was no successful treatment available for patients. Since then we have learned a great deal about trigger finger diagnosis and treatment.
Treatment of trigger fingers begins with conservative approaches. Some patients experience relief with use of oral anti-inflammatory medications (NSAIDs), topical anti-inflammatory creams, hand therapy, heating pads, and splints. Using a finger splint at night during sleep to keep the finger straight can relieve the condition in some patients. A corticosteroid injection (cortisone shot) is the most effective non-surgical treatment for trigger fingers. Most hand surgeons recommend trying one or two injections before considering surgery. It is not advisable to repeat the steroid injection many times, because detrimental effects to the soft tissues may occur. Diabetic patients should be aware that blood glucose levels can be elevated for a few days following steroid injections, and they should monitor their blood sugar closely.
Are cortisone shots bad?
Cortisone shots are not bad if used properly. One or two injections for a trigger finger is common practice in hand surgery. This practice does not result in long term problems. However, injecting corticosteroid into the same area multiple times is not recommended, because multiple doses of the medication can weaken the soft tissues, including ligaments, tendons, and joint cartilage. Additionally, it is usually advisable to delay trigger finger surgery at least 30 days following a cortisone shot in the finger to reduce the risk of infection and wound healing problems.
Is trigger finger surgery necessary?
Trigger finger surgery is typically recommended by hand surgeons if non-surgical treatment has not been successful at relieving a patient’s trigger finger symptoms. This is a common outpatient procedure which can be performed with local anesthesia (injected numbing medicine). Oral Valium or intravenous sedation are available for patients who have anxiety. During trigger finger surgery, surgeons often find thickening of the A1 pulley, enlargement of the tendon, and increased tenosynovitis (inflammatory tissue) around the tendon. Making an incision in the A1 pulley opens the sheath just enough to allow the tendon to move freely. This procedure usually fixes the problem. At the end of the surgery, it is common for the surgeon to assess the gliding of the tendons by asking the patient to make a fist. This step confirms that the finger is no longer triggering and the mechanical problem has been corrected.
In rare cases, simple A1 pulley release does not relieve the finger triggering. Additional sites of tendon triggering will need to be evaluated and further procedures may be necessary. For example, partial FDS tendon excision may be recommended to relieve the persistent triggering. In my practice, I see this approximately one or two times per year.
This is what a typical trigger finger surgery incision looks like (this incision would be for surgery on the middle finger trigger finger).

What are the complications following trigger finger surgery?
Complications following trigger finger surgery are not common. Our biggest concern is infection. Minor infections can be treated with wound care and oral antibiotics. Deeper infections into the tendon sheath are rare but are more complicated, often requiring revision surgery and a long course of antibiotics. Patients with diabetes, tobacco use, and compromised immune systems are more prone to infections. Other complications include stiffness, scar tissue, and limited finger range of motion. These complications can be treated with hand therapy and usually improve gradually over time. Damage to nerves and blood vessels is very rare and typically requires revision surgery. Recurrence of a trigger finger following successful surgery is not common.
What are the results from trigger finger surgery?
Most patients recover excellent finger range of motion and hand function within a few weeks of trigger finger surgery. The first two weeks after surgery are important to protect the hand from overuse and the incision from infection. It is ok to use the hand lightly and to gently move the fingers right away. Most patients can return to working at a computer or light duty work within a few days. 5 days following surgery, I allow patients to get the hand wet in the shower and clean it with soap and water in the sink. The incision should be kept clean and covered with a bandaid until the sutures are removed in about 2 weeks. Patients can resume heavier activities with the hand, such as weight lifting, gardening, and golf, as comfort allows starting 3-4 weeks after surgery. The majority of patients recover quickly after trigger finger surgery, and they are pleased with their results. On occasion, a patient develops joint pain, finger stiffness, and scar tissue which can slow down the recovery and take time to resolve.
This is a post-operative bandage following trigger finger surgery.

After 5 days following trigger finger surgery, patients can use this type of bandage:

For more information about trigger fingers, please make an appointment with a hand specialist.
Disclaimer: Please note, the material provided on this site is intended for general information only and does not constitute medical advice. This does not replace evaluation by a doctor. Please seek medical evaluation if you have a concern.
