Dupuytren Contracture is characterized by abnormal fibrous tissue formation in the palms of the hands and fingers. This fibrous tissue is very similar to the scar tissue of healing wounds in the body. Some patients also develop fibrous tissue in other parts of the body including the feet (Ledderhose disease), penis (Peyronie disease), and shoulder (adhesive capsulitis). Often Dupuytren disease begins with firm fibrous nodules in the palms. Over time these nodules can develop into cords which may draw the finger into a flexed position. If the finger is kept in a bent position for a long period of time, the joint becomes contracted and unable to fully extend and straighten. Joint contractures in the fingers may result in hand impairment. Some people notice difficulty performing everyday tasks with their hands, such as shaking hands, putting on gloves, reaching into a pocket, or playing a musical instrument.
Scar Tissue
Patients with Dupuytren contracture are predisposed to scar tissue formation in general. After surgery, the hand incisions heal with scar tissue. Early in the wound healing process, scar tissue is primarily made up of fibroblast cells and disorganized type 3 collagen. Gradually over several months, the scar tissue matures and becomes softer, thinner, and less red. In some Dupuytren patients this scar tissue can be thicker or harder than expected. Scar management techniques can be helpful to minimize scar tissue formation in the hand and maintain finger range of motion. These techniques include scar massage, use of cocoa butter with vitamin E moisturizer, hand splinting, silicone pads, and heat modalities. Night splinting is usually recommended for several weeks following surgery to maintain finger extension. Thick, firm, tight scar tissue can take several weeks or months to soften and smooth out. Hand therapists are usually very helpful in managing post-operative Dupuytren scar tissue.
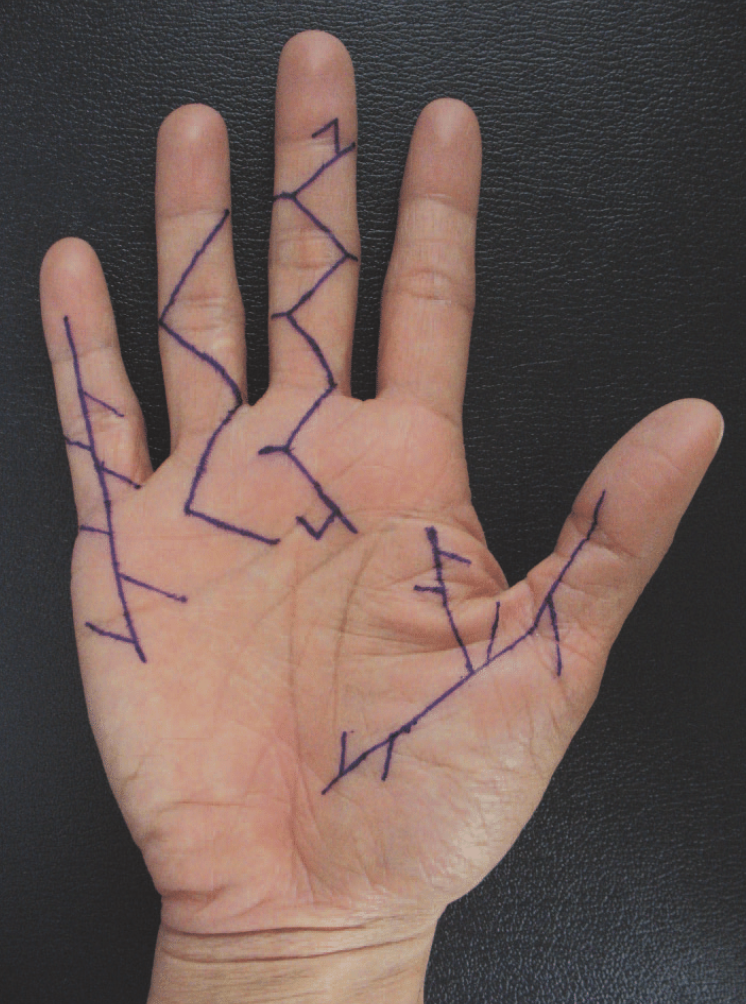
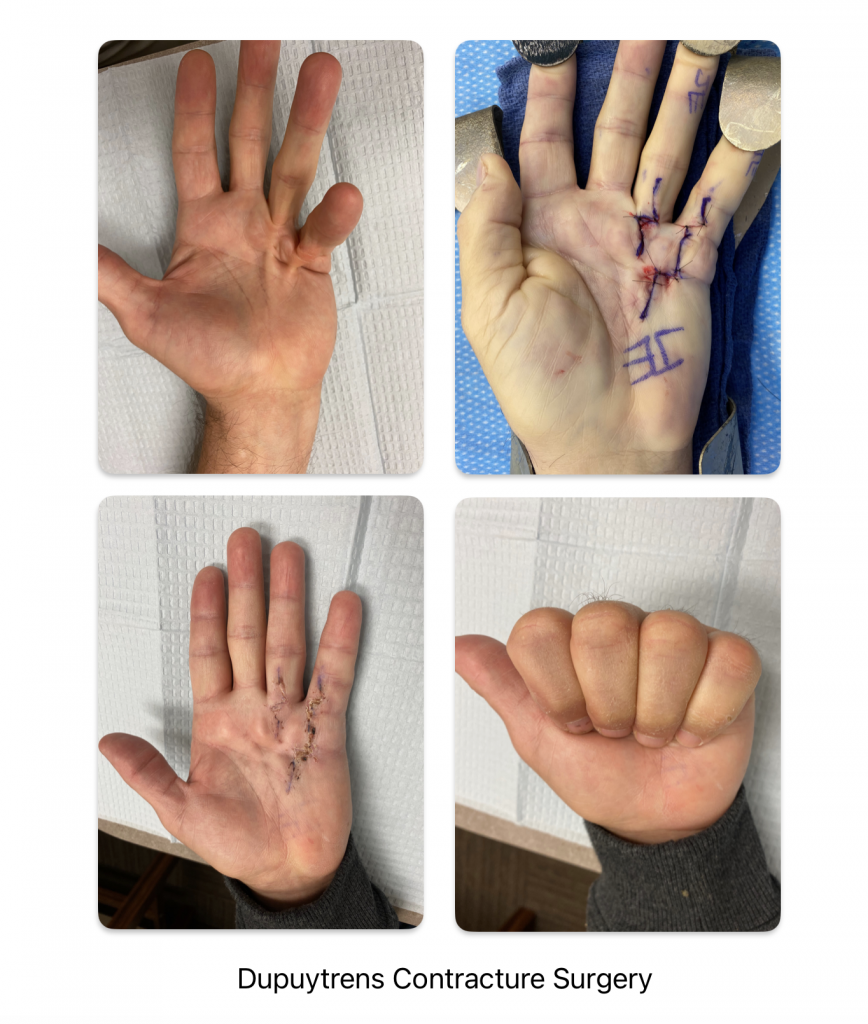
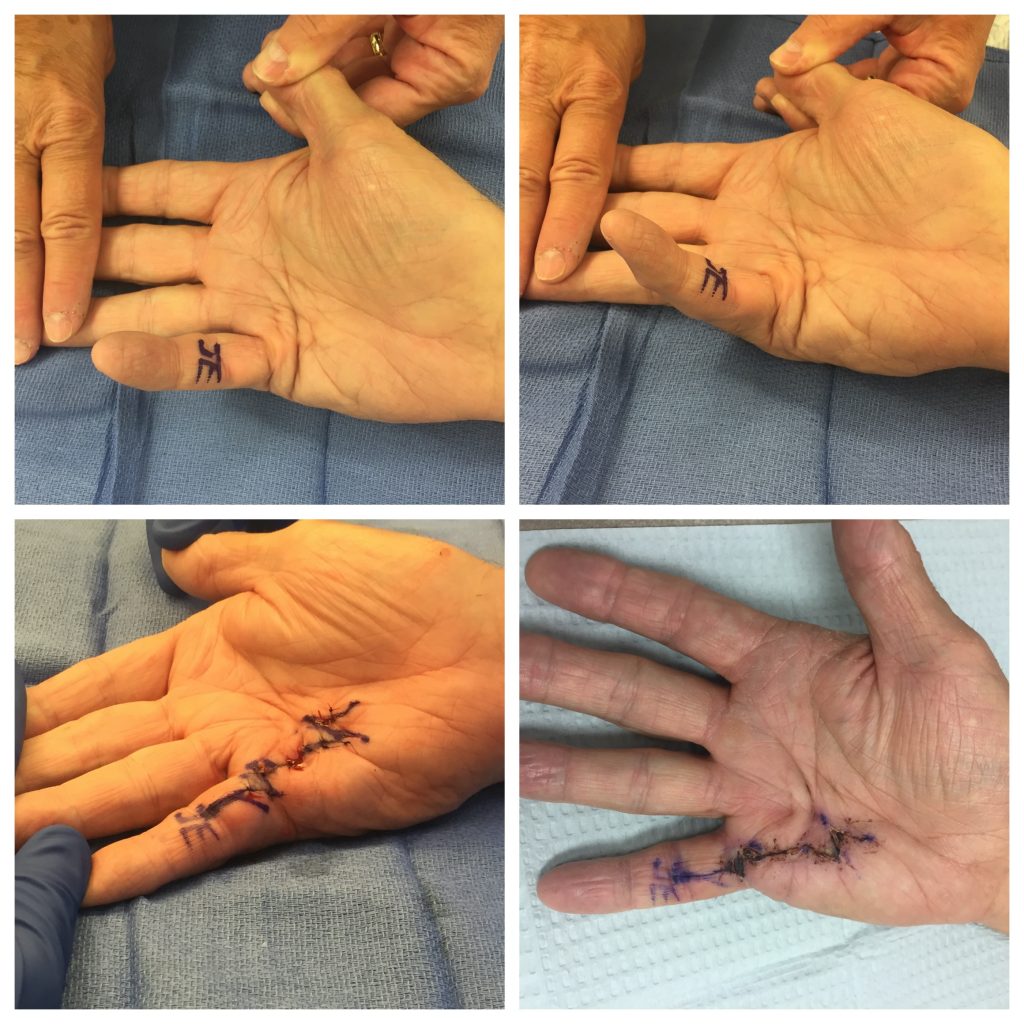
Dupuytren Contracture Surgery
There are many types of surgeries available for Dupuytren contracture. In the United States, many patients nowadays are treated with a limited fasciectomy surgery. The goal of this surgery is to remove only the Dupuytren tissue which is causing the finger contracture – not every piece of diseased fibrous tissue in the hand is removed. Think of this procedure as a surgical version of a targeted Navy Seal strike. This approach minimizes trauma to the rest of the hand, and minimizes swelling, stiffness, and scar tissue formation. Surgeons use various types of skin incisions to perform the procedure and often use a zig zag or z-plasty incision to allow the skin to have better mobility after surgery. Occasionally a skin graft is used to replace an area of unhealthy skin.
Hand Therapy after Dupuytren Contracture Surgery
Early initiation of hand therapy after surgery can help with the patient’s overall hand recovery. Hand therapists assist with wound care, finger range of motion, scar management, hand swelling, and hand strengthening.
Results after Dupuytren Contracture Surgery
No one wants to have surgery. However, the benefits of Dupuytren contracture surgery outweigh the risks in many patients. Good to excellent surgical results can be achieved for most patients, particularly before the contracture becomes severe. Most patients recover within a few weeks after surgery and are back to playing golf, lifting weights, and most hobbies about 4-6 weeks after surgery. Occasionally patients have swelling, stiffness, or scar tissue in their hands which delays the recovery several more weeks. The chance of Dupuytren contracture coming back in the same area is much lower with surgery compared to the non-surgical options. However, Dupuytren disease can still develop in the adjacent fingers or in the opposite hand, despite having surgery.
If you have Dupuytren contracture and have questions about your treatment options, please seek consultation with a hand specialist to learn more. Surgical and non-surgical options for Dupuytren contracture are available.
What is Dupuytrens’ Diathesis?
Patients with Dupuytren’s diathesis have a strong predisposition for developing severe joint contractures as well as recurrent disease after treatment. The word diathesis means “predisposition” or “tendency.” Dupuytren’s diathesis is classically seen in patients who develop Dupuytren at a young age, such as in their 40s, have a strong family history of Dupuytren, and have fibromatosis at other locations in the body. These patients should be advised that they have a higher risk of joint contractures in their hands than the average patient.
What are risk factors for Dupuytren contracture?
Genetic risk factors for Dupuytren contracture include Northern European ancestry, family history, and male sex. Environmental risk factors for Dupuytren contracture include smoking, alcohol abuse, diabetes, some seizure medications, and hand trauma.
