Carpal tunnel syndrome (CTS) is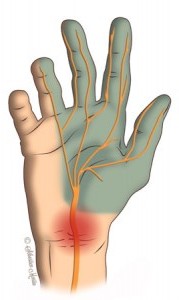 the most common nerve problem in the arm. It results from increased pressure on the median nerve at the wrist, within the carpal tunnel. Carpal tunnel syndrome is a type of “pinched nerve.” The symptoms are usually worse at night and can wake patients up from sleep.
the most common nerve problem in the arm. It results from increased pressure on the median nerve at the wrist, within the carpal tunnel. Carpal tunnel syndrome is a type of “pinched nerve.” The symptoms are usually worse at night and can wake patients up from sleep.
The word “carpus” is derived from the Greek word karpos, which means “wrist.” The carpal tunnel is a passageway in the wrist through which the median nerve and tendons of the hand travel. The carpal tunnel is a narrow, confined space: the floor of the tunnel is made up by the carpal bones of the wrist, and the roof is created by the transverse carpal ligament. The median nerve is at risk for compression within this tunnel. If there is abnormal swelling, abnormal wrist anatomy, or injury to this area, median nerve function may be affected. Patients may experience symptoms such as numbness, tingling, weakness, and pain in the hand. The median nerve gives sensation to the thumb, index, middle, and half of the ring finger. The median nerve also controls most of the muscles in the thumb (thenar muscles).
What causes carpal tunnel syndrome?
In most cases, the cause of CTS is unknown. Diabetes, thyroid disorders, rheumatoid arthritis (RA), pregnancy, vitamin deficiencies, and fluid retention can be associated with CTS. Wrist fractures and swelling of the flexor tendons can cause carpal tunnel syndrome. Women are more commonly affected than men. Repetitive forceful gripping and heavy use of vibratory tools may increase a person’s risk of CTS.
How do I know if I have carpal tunnel syndrome?
Patients with CTS commonly report numbness, tingling, and pain in the hand and fingers. The thumb, index, and middle fingers are usually affected the most. Some patients notice that the hand feels cold, swollen, “asleep” or describe “poor circulation” in the fingers. Symptoms can awaken patients at night with “pins and needles” tingling hand pain, and patients tend to shake their hands for relief. Some patients report increased symptoms while gripping a steering wheel or reading a book in bed. Initially symptoms come and go, but over time the numbness can become constant. Dropping objects or having a weak grip are also common complaints. In severe or long-standing cases, the muscles at the base of the thumb (thenar muscles) can become weak and atrophy.
Often the diagnosis can be made on the basis of your symptoms, medical history, and physical examination. During the office visit, I routinely examine the neck, shoulder, elbow, wrist, sensation in the hand, and muscle function in the hand. I also test the irritability of the median nerve. This involves tapping along the course of the nerve (Tinel’s test), holding the wrist flexed (Phalen’s test), and gently pressing on the carpal tunnel (carpal compression test). A nerve test (nerve conduction study NCS and/or electromyogram EMG) can be used to confirm the diagnosis.
Not all hand pain or numbness is caused by carpal tunnel syndrome. The nerves of the arm can be compressed or “pinched” anywhere along their pathway from the cervical spine (neck) to the fingers. Therefore it is important to identify the location of the nerve compression.
What are the treatment options for carpal tunnel syndrome?
Not everyone with carpal tunnel syndrome needs surgery. Fortunately, many people with CTS improve with non-operative treatment. Many people sleep with the wrist bent, which puts more pressure on the median nerve. Wearing a wrist brace at night supports the wrist in neutral alignment and takes pressure off the nerve. Modifying daily activities – particularly avoiding prolonged wrist flexion, forceful and repetitive gripping or vibratory tools – may help. Corticosteroid injections in the carpal tunnel (“cortisone shot”) provide an anti-inflammatory effect and can be effective in many patients. Some patients may benefit from tendon gliding exercises, range of motion exercises, and stretching programs. Taking B6 vitamin supplements may also help some patients.
If this does not help, or if nerve compression is severe, surgery may be recommended. A carpal tunnel release (CTR) is performed to decrease pressure on the median nerve. During this procedure, the “roof” of the carpal tunnel (transverse carpal ligament) is divided through an incision at the base of the palm. Cutting the transverse carpal ligament increases the size of the carpal tunnel and provides more room for the median nerve.
What is the recovery from carpal tunnel surgery?
Carpal tunnel surgery is performed in Raleigh as an outpatient procedure usually under local anesthesia (numbing medicine). Patients may use their hands for light activities immediately, and I encourage gentle finger and thumb range of motion. Most people can return to light duty work in a few days. Normal use of the hand is resumed as comfort permits. Pain medication is often weaned in a few days. The soft surgical bandage can be removed after about 5 days. Afterwards the wound should be covered with a large band-aid and kept dry. The skin sutures are removed in clinic in 10-14 days. Most patients do not require physical therapy or a brace after surgery. I recommend avoiding heavy lifting, pulling, pushing or gripping for approximately 3-4 weeks after surgery.
What are the results from carpal tunnel surgery?
Most patients are satisfied with their result after carpal tunnel surgery. Many patients report improvement in their numbness, tingling and pain in just a few days, but others may take longer to heal. Some patients do not have complete relief of symptoms, especially in severe or long-standing cases. In some severe cases, the nerve may not recover and the numbness does not improve, even with surgery. Soreness in the palm at the incision is common after surgery for several weeks.
Endoscopic vs. open carpal tunnel surgery
When a patient is planning to under carpal tunnel surgery, there are several types of surgeries available. These include traditional open release, mini-open release, and endoscopic release. Hand surgeons continue to debate the pros and cons of each technique. The various techniques have been compared in scientific studies, and the long-term results and complication rates are similar between the procedures. Less-invasive techniques result in less pain in the short-term than the traditional open approach. The most important aspect of the procedure is releasing the transverse carpal ligament while avoiding complications. Surgeons use the procedure that has worked well in their hands, which they know they can perform safely.
I have used 
I advise patients to use their hand lightly over the next 2-3 weeks and “let pain be your guide” on gradually increasing activities. Stitches are removed in the clinic about 10-14 days post-op. After surgery, most patients are pleased with the improvement in the numbness and painful tingling symptoms. Surgical-site pain and scar tenderness gradually decrease over a few weeks. Most patients regain function and range of motion on their own without formal hand therapy.
